- Panels
Product Links
Try Simplicity Panel™ today by requesting a physical demo box to be mailed to your lab.

- Collection
________________________________________

Molecular Designs offers an innovative Opti-Swab Liquid Amies Transport System. This advanced solution enables reliable collection and transport of a wide range of viral and bacterial pathogens, making it suitable for various testing applications.
State-of-the-art nylon flocked nasopharyngeal and oropharyngeal swabs designed with improvements to specimen collection and diagnostic reliability in mind.

.png?width=200&height=200&name=Scribble%20(14).png)
- Extraction
A novel nucleic acid extraction system that leverages magnetic bead technology to automate the extraction process. This innovative solution lets labs perform extractions faster, at a lower cost, and more accurately.

- LIS
- Resources
- About Us
- Contact us
- FAQ
- Lamda Biotech
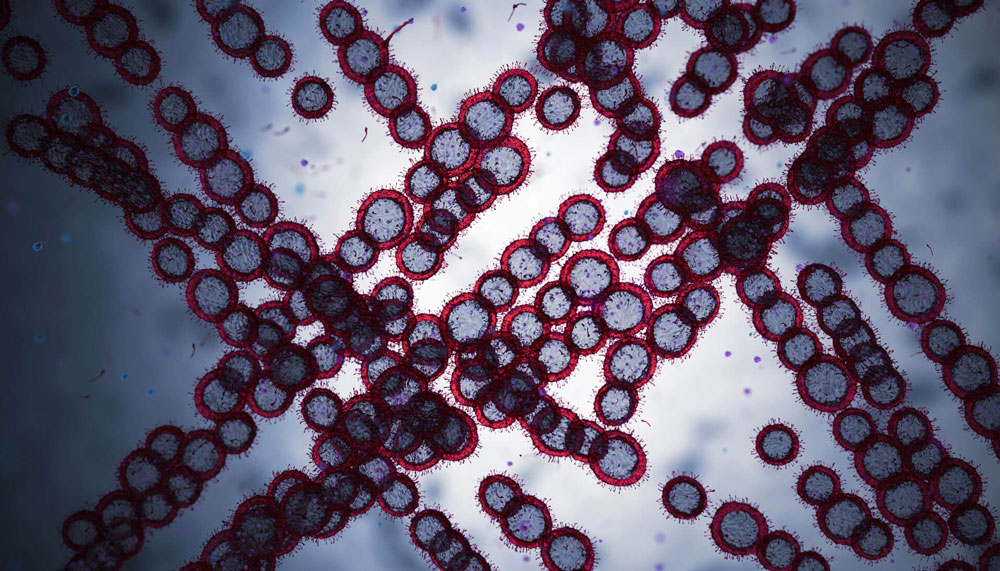
Candida Auris: Responding to the Emerging Threat
Contents
If there is one accomplishment that stands above all else in the history of modern medicine, it is its triumph over infectious disease. And while the rise of pathogen-specific antibiotics and advances in diagnosis are our crowning achievements, the war is not fully won. Worldwide events like the COVID-19 pandemic have made this painfully obvious, but it is also a reality we confront with less-notorious pathogens like Candida auris.
Candida auris was first isolated in 2009 when a 70-year-old woman in Tokyo sought treatment for an ear complaint.1 Since then, the fungus has spread to five continents. In 2017, only 112 cases were reported2, but by 2021, the United States reported over 1,460 cases, 3 highlighting its rapid spread.
While C. auris primarily affects immunocompromised and other critically ill patients, it has become a subject of intense scrutiny due to its high mortality rate, tendency to spread quickly in inpatient environments, and high level of resistance to multiple drugs and empiric therapies.
Increasingly Universal Approaches to Screening and Testing
Considering its recent appearance on the medical community’s radar, reactions to C. auris have been mixed. At the federal level, the Centers for Disease Control and Prevention (CDC) has taken proactive measures in the form of guidelines for the screening, testing, and containment of C. auris in healthcare facilities, where it is most prone to spread. Additionally, the CDC provides for free testing of C. auris colonization screening through their AR Lab Network. The CDC also performs comprehensive tracking of C. auris outbreaks and makes this information publicly available.
At the state level, public departments of health are increasingly recommending rigorous screening and testing programs. As early as 2016, New York State implemented mandatory reporting of C. auris. California has issued state-wide guidelines on C. auris screening and works closely to provide resources to help facilities respond to the threat.
In Texas, healthcare systems have implemented a tiered approach to screening and some larger healthcare systems within Texas have invested in advanced laboratory technology to expedite the detection of C. auris, allowing for more rapid isolation and treatment of affected patients. Because of the groundwork laid by states like these, as of 2023, 22 states require state-level reporting of Candida auris.
Common Screening Protocols
While this varies with locale, screening criteria typically include recent hospitalization (especially abroad), recent surgery, prolonged stays in long-term care facilities, and previous colonization or infection with C. auris. Screening tests are typically conducted using swabs of various body sites, such as axilla and groin, where the fungus is more likely to colonize.
The CDC themselves recommend PCR as first-line for diagnostic confirmation considering its accuracy and speed, with cultures as a second choice. In many states, reporting of C. auris is mandated should it be discovered.
Candida Auris in the Literature
A review of recent literature related to C. auris can appear bleak. In addition to its alarming spread rates, one recent paper illustrated an increasing resistance to echinocandins like caspofungin, micafungin, or anidulafungin, which are considered the first-line treatment for Candida auris infections.4
Other troubling findings are related to the mortality rate. As an infection which primarily affects immunocompromised and critically ill individuals with comorbidities, it can be difficult to pin the mortality rate down, but it is estimated to be between 30 and 60%.5 A 2023 CDC report analyzing 192 hospitalizations associated with Candida auris uncovered an estimated crude mortality rate of 34%.6
While resistance to echinocandins is increasingly being reported, one popular agent (micafungin) is estimated to be 86% effective at treating cases.7 Novel echinocandin agents are being developed and recommended, like rezafungin8 and anidulafungin.9
Early Detection and Treatment
Considering the rapid spread of C. auris in healthcare facilities and its responsiveness to early detection and treatment, it is obvious that clinical diagnostic laboratories’ ability to rapidly respond to the threat is critical. Of course, this is evident at the level of the individual patient, but it is also a great example of how individual labs can use the power of speed and accuracy to prevent the spread of a lethal illness at the population level.
For these reasons, waiting days for a culture to return is not a feasible option when C. auris is suspected or where increasingly-common rigorous screening programs are implemented. While PCR has been around for many years, its use during the COVID-19 pandemic cemented the platform not only as a way of obtaining diagnostic labs quickly (within 2 hours), but also as one with high levels of sensitivity and specificity.
At Molecular Designs, we’re applying the power of PCR to the challenge that C. auris presents the diagnostic community. We are currently in the process of developing a PCR panel that can detect Candida auris so labs and providers can more effectively respond to the danger posed by this fungus. It is in this way we hope to contribute to the healing and protection of individual patients and the broader community.
References:
- Gorvett Z. The mystery origins of Candida auris - BBC Future. BBC News. Published March 31, 2023. Accessed April 26, 20231
- Candida auris—a mysterious and tenacious enemy. National Institute of Allergy and Infectious Diseases. Published September 23, 2022. Accessed April 26, 2023
- Sharon Tsay, Alexander Kallen, Brendan R Jackson, Tom M Chiller, Snigdha Vallabhaneni, Approach to the Investigation and Management of Patients With Candida auris, an Emerging Multidrug-Resistant Yeast, Clinical Infectious Diseases, Volume 66, Issue 2, 15 January 2018, Pages 306–311, https://doi.org/10.1093/cid/cix744
- Thatchanamoorthy N, Rukumani Devi V, Chandramathi S, Tay ST. Candida auris: A Mini Review on Epidemiology in Healthcare Facilities in Asia. Journal of Fungi. 2022; 8(11):1126. https://doi.org/10.3390/jof8111126
- Egger NB, Kainz K, Schulze A, Bauer MA, Madeo F, Carmona-Gutierrez D. The rise of Candida auris: from unique traits to co-infection potential. Microb Cell. 2022 Aug 1;9(8):141-144. doi: 10.15698/mic2022.08.782. PMID: 35974811; PMCID: PMC9344200.
- Benedict K, Forsberg K, Gold J, et al. Candida auris‒Associated Hospitalizations, United States, 2017–2022. Emerging Infectious Diseases. 2023;29(7):1485-1487. doi:10.3201/eid2907.230540.
- Cândido ES, Affonseca F, Cardoso MH, Franco OL. Echinocandins as Biotechnological Tools for Treating Candida auris Infections. J Fungi (Basel). 2020 Sep 22;6(3):185. doi: 10.3390/jof6030185. PMID: 32971857; PMCID: PMC7558506.
- Christopher L Hager, Emily L Larkin, Lisa A Long, Mahmoud A Ghannoum, Evaluation of the efficacy of rezafungin, a novel echinocandin, in the treatment of disseminated Candida auris infection using an immunocompromised mouse model, Journal of Antimicrobial Chemotherapy, Volume 73, Issue 8, August 2018, Pages 2085–2088, https://doi.org/10.1093/jac/dky153
- Vazquez JA, Sobel JD. Anidulafungin: a novel echinocandin. Clin Infect Dis. 2006 Jul 15;43(2):215-22. doi: 10.1086/505204. Epub 2006 Jun 9. PMID: 16779750.




